News from QED Bioscience
ELISA: How I Wonder What You Are
My phone’s email notification went off, and I rolled over in bed to look at the clock. Saturday, 5 am. Wonderful. Who would email me at that hour? It had to be my undergraduate research PI. I unlocked my phone. Yep. Doesn’t he ever sleep?
Dear Casey: We are launching a new collaborative project in which we will be measuring human albumin levels in serum of control patients and comparing those with patients suspected to have decreased albumin levels. We will be measuring albumin levels using ELISA. I need an assay plan drawn up and submitted to me by 5:00 today.
Wow, he had me as the lead on this project! Now all I needed to do was get into the lab and figure out who Elisa was and how she was going to help me on this project!
Starting Out: Enzyme-Linked Immunosorbent Assay
Having gotten to the lab and done some preliminary digging, I was disappointed to find out that Elisa would in fact not be helping me on this project. As it turns out, “her name” is an acronym for Enzyme-Linked Immunosorbent Assay, or ELISA.
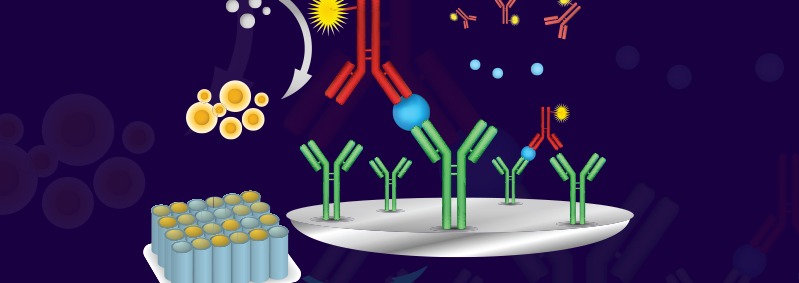
I discovered that an ELISA uses antibodies that bind to their respective target antigens on an ELISA plate, and it includes antibodies that are linked to an enzyme that converts a substrate into a colored product when the target antigen is present. More target means more color. Simple enough, right?
Planning, Planning and More Planning – Indirect, Direct, or Sandwich ELISA??
To plan the study, I needed to make some big decisions. First, what kind of ELISA did I want to run? There are many permutations of this assay (including an indirect ELISA described here), but I narrowed it down to two options: a direct ELISA or a sandwich ELISA.
1. Direct ELISA
A direct ELISA involves coating the plates with a mixture containing the target analyte – in this case, patient serum. With this setup, I could use a conjugated anti-albumin antibody to detect the presence of albumin. Alternatively, and to enhance the signal, I could use an unconjugated anti-albumin antibody followed by a secondary, enzyme-conjugated detection antibody. The downside to the direct ELISA is the fact that albumin only makes up a small percentage of serum, thus only a small percentage of the plate would be coated with albumin. This didn’t seem like the way to go with patient samples potentially containing decreased albumin levels.
2. Sandwich ELISA
The other option was a sandwich ELISA. This technique involves coating the plates with a capture antibody first; in this case an anti-albumin antibody. After adding patient serum to the plates, a second anti-albumin detection antibody would be used to detect the presence of albumin. Using this technique, the albumin would be enriched in the well by the coating antibody. This seemed like the best bet to detect albumin in potentially albumin-deficient patients.
Having decided upon the sandwich ELISA format, I planned further ahead and made several decisions along the way, as outlined below.
1. Plate Selection and Coating
The first steps of any ELISA involve coating the plate, and this requires two decisions:
I. What type of plates was I going to coat?
II. What was I going to coat plates with?
The main thing I kept in mind for the first decision was to order plates specially designed for ELISAs. These plates are made of polystyrene and typically have 96 clear, flat-bottomed wells. The wells also carry a net charge on their surface to interact with and bind to proteins. I was warned that choosing the wrong plates is a common pitfall. Mistaking a tissue culture plate for an ELISA plate is an honest enough error, but as tissue culture plates lack the requisite charge, mixing these up will produce an ELISA with minimal signal, if any at all.
Regardless of what I was actually putting on these plates, I needed to make sure I was diluting it in coating buffer before adding it to the plates. Coating buffer is typically carbonate-based and has a high pH (between 9.5 and 10) to surpass the pI of the protein and induce a net charge across the surface. The net charge of the protein then interacts with and binds to the charged plate surface. To ensure maximum coverage of the plate surface, I decided to use a concentration of 10 µg/ml coating antibody (anti-albumin antibody), but often the optimal concentration of the coating antibody is determined by testing a range of antibody concentrations.
2. Blocking
A fellow student mentioned that it was not safe to assume that the coating antibody would occupy all of the binding surfaces on the wells. I would need to prevent my detection antibody sticking non-specifically to any unoccupied surfaces that would give me an artificially high signal (i.e. high background). I could achieve this by adding a blocking buffer after applying the coating antibody. This blocking solution should contain an irrelevant protein that my detection antibody would not bind to. A solution containing BSA (bovine serum albumin) is commonly used for this purpose, but bovine serum albumin might not be my best bet, as anti-human albumin antibodies might bind to bovine albumin. Instead, I went with a 5% milk solution in TBS or PBS (with a small amount of detergent for added specificity).
3. Antibody Selection
Another critical planning step involved deciding what type of antibody I wanted to use. Specifically, I needed to understand the implications of using monoclonal antibodies vs. polyclonal antibodies in ELISAs.
Monoclonal antibodies are produced by a single B-cell clone producing an antibody against a single epitope on an antigen. To use monoclonal antibodies in ELISA, two antibodies having different epitope specificities would be needed. One antibody would coat the plate, thus immobilizing any albumin present in patient samples to the plate, and a second antibody (conjugated to an enzyme) that recognizes a different epitope, would detect the presence of albumin and produce a detectable signal. However, monoclonal antibodies might not be ideal if the epitopes they recognize are not present in high enough concentrations to be detected.
Polyclonal antibodies, on the other hand, are mixtures of antibodies produced by a number of different B-cells against several epitopes present on one target protein. Whereas a monoclonal antibody against albumin would bind to a single albumin epitope, a polyclonal antibody mixture could potentially bind to multiple epitopes on albumin. I decided that a polyclonal antibody would be most optimal for my ELISA setup for the following reasons:
- Because polyclonal antibodies bind to multiple epitopes, a single polyclonal antibody could be used to coat the plate and immobilize the albumin, and the same antibody could be conjugated to an enzyme to act as the detection antibody.
- Furthermore, the ability to bind multiple epitopes allows polyclonal antibodies to bind to multiple sites on the albumin, significantly amplifying the signal produced by a single albumin molecule.
- Finally, polyclonal antibodies can be used to detect both native and denatured proteins since they are not restricted to recognizing a single epitope that may be dependent upon intact tertiary structure.
4. Washing
Washing plates after each incubation step is required in ELISA to prevent non-specific interactions. I was advised to wash the plates using TBS or PBS (with a small amount of detergent) after all antibody incubation steps.
5. Detection and Development
There are a myriad of different detection methods available with ELISA, but by far the most common is the use of an antibody conjugated to an enzyme called horseradish peroxidase (HRP). This enzyme produces a blue color when exposed to one of its substrates, e.g. 3,3’,5,5’-Tetramethylbenzidine (TMB). The reaction can be stopped (i.e. color development halted) by adding an acid (typically sulfuric acid), which converts the substrate from a blue to a yellow color.
6. Reading
The intensity of the color signal is typically read on a spectrophotometer set to a wavelength that’s appropriate for the substrate used. Many automatic plate readers are set up to read an entire 96 well plate in one reading, storing the data in an organized manner.
To determine the concentration of albumin in my patient samples, I first had to prepare a standard curve. The standard curve is created by reacting a series of known concentrations of the target analyte (in this case, albumin) in the ELISA set-up I was going to use. The resulting OD (optical density) values obtained typically form a sigmoidal (S) curve reflecting the upper and lower limits of the ELISA (See Figure 1). The X-axis, which represents the known concentrations of the target analyte, may be presented as a log-scale, to prevent “clumping” of data points on the lower end of the curve. The Y-axis represents the OD values obtained with each concentration of analyte.
I could then extrapolate the concentration of albumin in my samples from the standard curve by finding the concentration corresponding to the absorbance values I obtained. I was told by a lab-mate that it was wise to carefully determine the optimal sample dilution range, as this is another common pitfall! It’s easy to run an undiluted sample and generate a data point with very high absorbance and extrapolate from the standard curve to meet that data point. However, once the ELISA signal becomes saturated, it is not possible to distinguish between different concentrations. Quantitation is most accurate in the linear portion of the standard curve, so if your sample needs to be diluted 5-fold to be in that range, just determine that concentration and multiply by 5 to determine the concentration in the original sample.
Armed with a well thought out ELISA protocol, I got the proposal submitted to my PI and started looking forward to another night in bed. Hopefully there won’t be another 5 am wakeup call!